Dr Tim Senior, a GP and a contributing editor at Croakey, recently took the reins of @WePublicHealth to share some of his findings from a Churchill Fellowship investigating GPs and primary care teams working in marginalised communities in the United Kingdom and Ireland.
His posts, summarised below, highlight the importance of values, collegiality, innovation, compassion, creativity, and singing for happiness and health.
Tim Senior writes:
I’ll start by acknowledging that even though I’m on the other side of the world at the moment, I live and work on Dharawal country in the land often known as Australia, and that sovereignty has never been ceded.
I’m a GP. I work in Aboriginal Community Control (a NACCHO service), and have been at the same service for nearly 20 years now. I also do some work at the Royal Australian College of General Practitioners in Aboriginal and Torres Strait Islander Health, Standards and health equity.
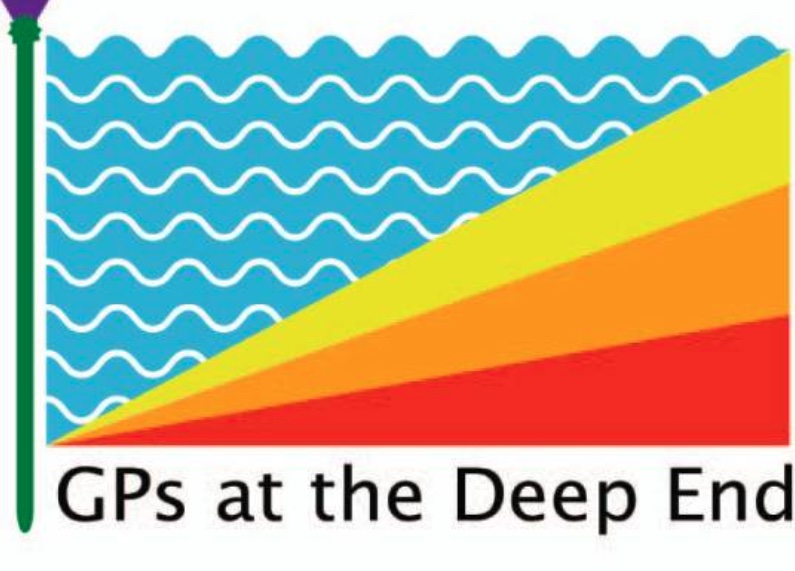
You’ll hear me use the term “Deep End” a lot this week. What is the Deep End?
Back in 2011, I’d been working as a GP in Aboriginal health for 7 years, working with people with a complex mix of multiple medical problems, difficult social circumstances, often causing mental health problems, on a background of trauma…and then I read this article in The British Journal of General Practice, GPs at the Deep End.
They called themselves Deep End GPs. They were describing the work of GPs in the 100 most deprived communities in Scotland.
Over the next year they published a series of articles describing their work, which are collected together as an RCGP Occasional Paper (available here).
There was I, on the other side of the world, working in an Indigenous community, and yet these GPs in Glasgow were describing exactly the work I was doing. It turned out I was a Deep End GP!
Deep End explainer
This set me on a path of understanding more fully the interaction of poverty on Aboriginal and Torres Strait Islander health and on health in rural and remote communities, and ultimately led to my Churchill Fellowship.
This is the original Deep End logo, and explanation. The logo represents that workforce (in fact, resources) are spread evenly, even though need for those resources is not.
GPs at the Deep End are treading water, with insufficient time to get to the bottom of patients’ problems. See also this article published by the British Medical Association, Deprivation meets inspiration.
Add to that multimorbidity, complex social circumstances requiring lots of forms for housing, welfare (along with the unfair treatment in those systems), lack of money restricting choices around food, air quality, and the consequent mental health problems…You can see why patients and GPs feel like they are just treading water. Hence, the Deep End.
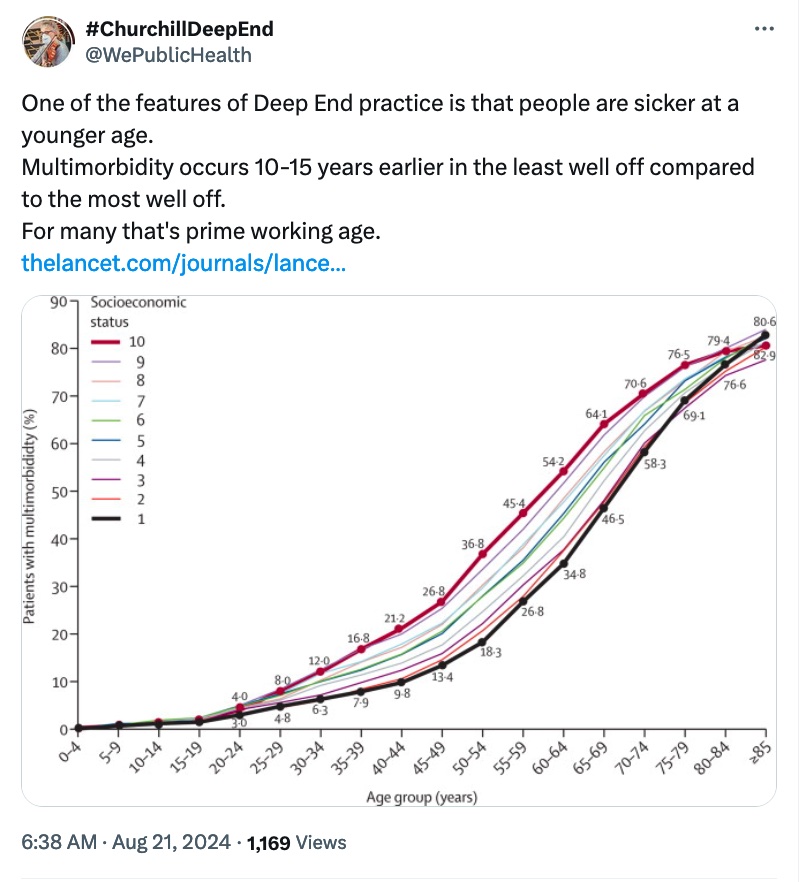
I really think we need to remember this when we talk about the aging population. If we’re thinking about the health needs due to aging hitting in 10 to 15 years’ time, that’s happening *right now* in deprived communities (see this 2017 article, Ageing meets unequal population).
Also, as a fine example of the distribution of resources, have you come across the Red Rooster Line in Sydney?
As a GP, I can be sat in a consultation advising about healthy eating, but, because of cost and geography, it’s not available to my patients. And that’s just in the city. You’ve seen the cost of fruit and vegetables in remote communities, yes? “…via the unconditional, personal continuity of care provided for all patients.” Really strong evidence now about the effect of continuity on health outcomes. Such good evidence that it would be approved by the TGA and on the PBS in no time if it was a drug.
“…via the unconditional, personal continuity of care provided for all patients.” Really strong evidence now about the effect of continuity on health outcomes. Such good evidence that it would be approved by the TGA and on the PBS in no time if it was a drug.
“…whatever condition or combination of conditions they present.” You might be starting to think of Starfield at this point! Managing the problems people present with. No wrong door. No referral criteria. Just trust and reducing harms, also taking opportunities for prevention
“The contribution of general practice to improving health and narrowing inequalities in health is not so much via the learning of new tricks and delivery of externally devised toolkits as by *increasing the volume and quality of what Deep End practices do.*” Read that again.
I cannot tell you how many times GPs have been told what we *should* be doing, how many times we’ve been given another toolkit, how many times we’ve been offered another webinar to fix a perceived deficit in our practice. No, really.
For the vast majority of things GPs do that frustrate you that you think we should do better, there is a systemic reason, rather than something we don’t know, or that we just have a personality failure. Really.
Introductions
Meet the GPs who contributed along the way.



 As well as the general practice, in the same building is special care dentistry (for those with anxiety, neurodivergence etc) and third sector community agencies.
As well as the general practice, in the same building is special care dentistry (for those with anxiety, neurodivergence etc) and third sector community agencies.
For the people
 Healing arts
Healing arts
We had a mindfulness workshop with a string quartet from the Scottish Ensemble (which made me realise I haven’t played viola in 2 months, and I’m really missing it! Again, the beneficial effects of participation!) P.S. The first violinist is Australian!
I did learn a new skill! Not dancing. (Those who know me know how unlikely that would be!) No, I learnt how to DJ! Albo, I’m coming for you! (I really enjoyed this, by the way. Again, the beneficial effects of participation, whatever it’s in).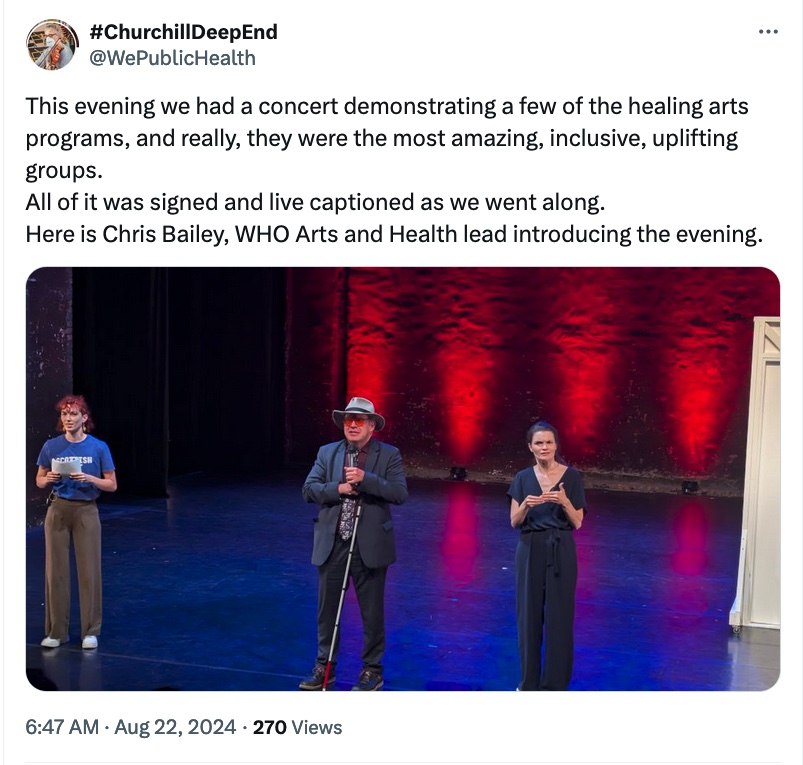
 El Sistema has the motto “music for social change”.
El Sistema has the motto “music for social change”.
Here are some of the Glasgow City of Poets, who had created poetry just today from words brought by participants in today’s conference.
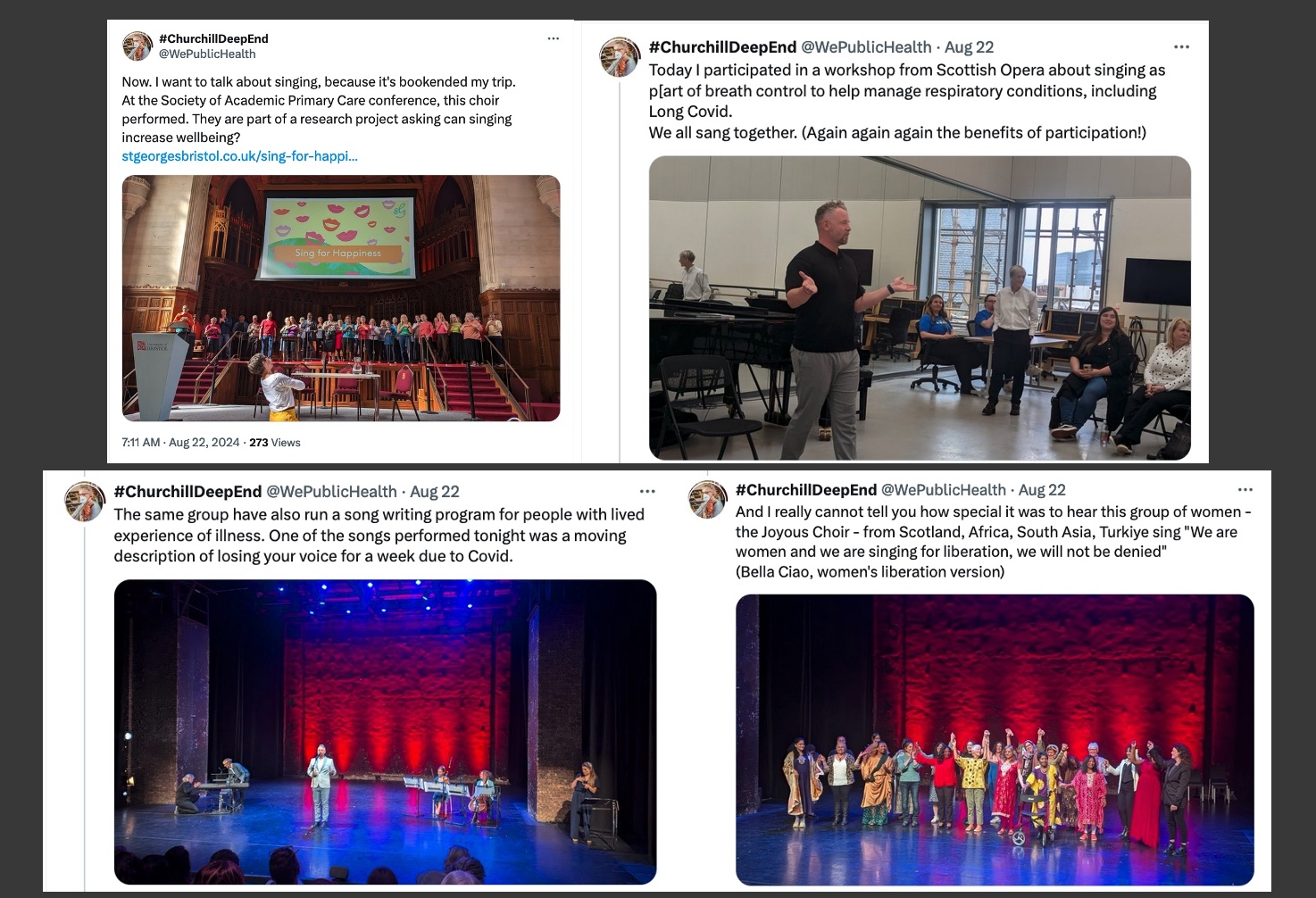
I’ve been to conferences where I have seen and participated in singing workshops with @IsabelJHanson and @drhesterwilson and I think if you don’t have a singing workshop at your conference, you’re not doing your conference properly. Seriously. Conference organisers, get on it!
Gardens matter

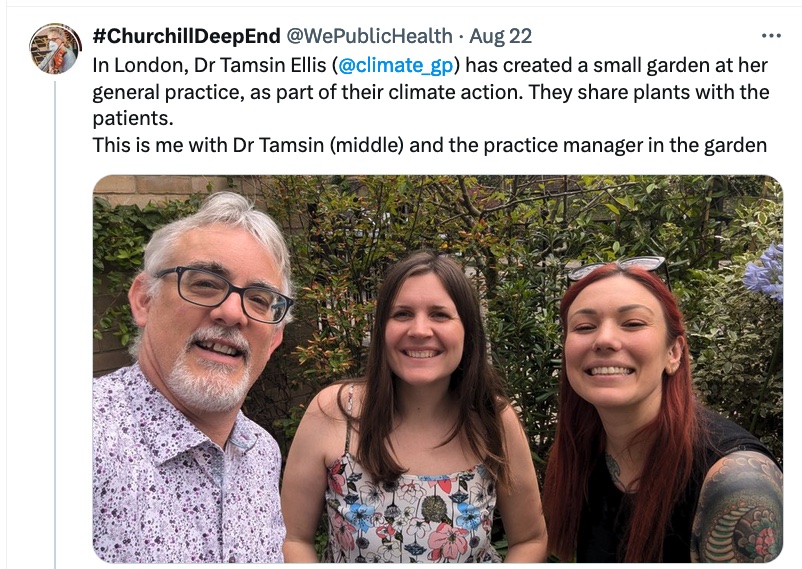 There’s a long list of things the practice is doing to make themselves more environmentally sustainable. But the thing is, each of these is achievable. And it wasn’t all done at once. Just starting, then improving.
There’s a long list of things the practice is doing to make themselves more environmentally sustainable. But the thing is, each of these is achievable. And it wasn’t all done at once. Just starting, then improving.
Of note, their values aren’t just a statement: “We ask staff to reflect on how they have helped sustainability as part of our appraisals and interview process Green Impact is a standing item on agendas for meetings. We regularly ask our staff to feedback ideas for improvement.”
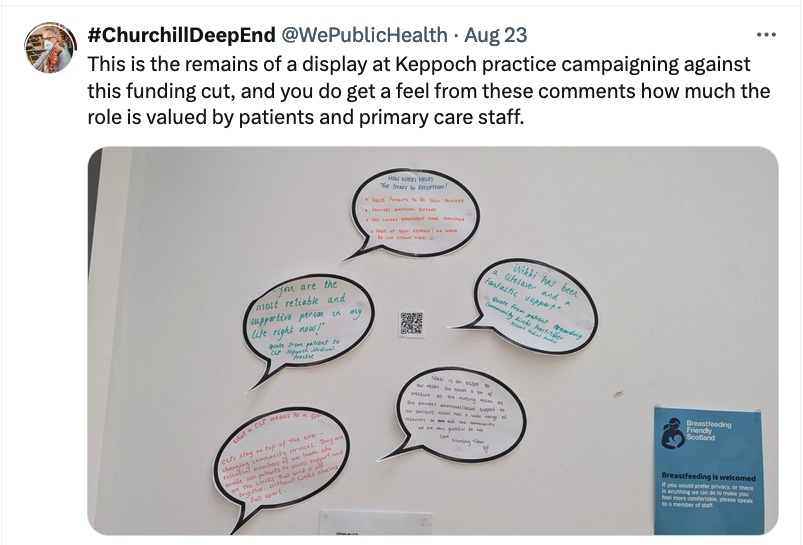
 Community Links Workers
Community Links Workers
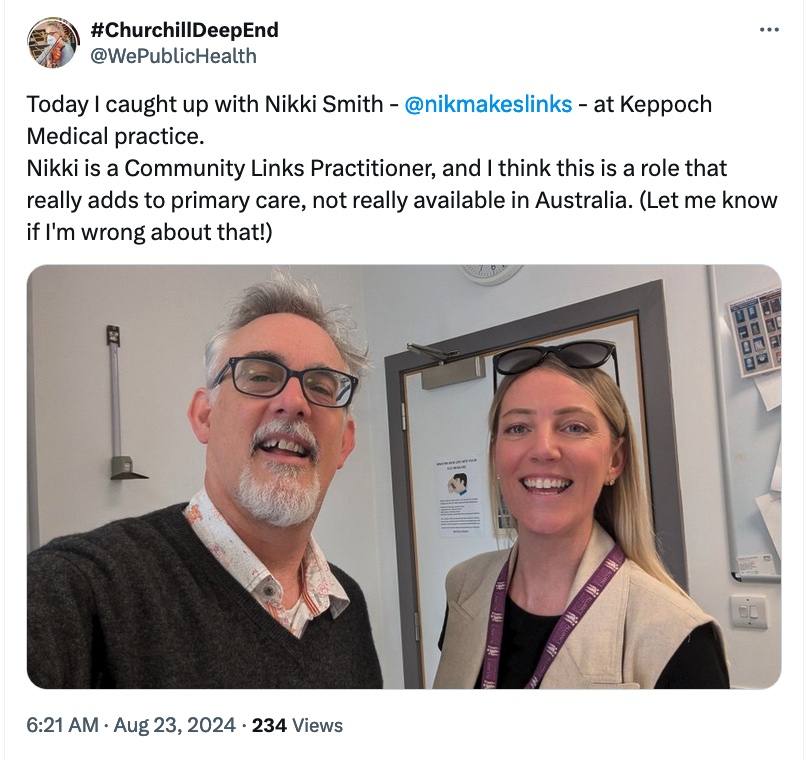 Speaking to Nikki Smith today, I was thinking about many of my patients, and I’d fill up her referral list easily in a day or two!
Speaking to Nikki Smith today, I was thinking about many of my patients, and I’d fill up her referral list easily in a day or two!
Community Links Practitioners have been placed in the most deprived general practices in Scotland specifically to act locally with individual patients and families in mitigating the social circumstances that worsen health.
Community Links Practitioners are placed in general practices, and are part of the primary care team, but they are employed by the Health and Social Care Alliance Scotland.
There are three components to the role:
1. Seeing patients of the practice to provide pragmatic assistance, depending on what they need. CLPs can guide people to help with social isolation, exercise, activities, help with housing and welfare.
2. “Community asset mapping” – they find out what community resources are available in an area, and establish relationships with them, and can even help getting some funding at times.
3. Meetings with other Community Links Workers that provide peer support, share advice and resources, and provide learning and education. Now, policy makers and funders will always want to cut this part. It’s not seeing patients, so surely it’s just inefficient! No, no, and a more resounding NO! This peer support and sharing education and resources is really crucial to the role.
You can read more about the Community Links Workers here.
The closest role we have to a Community Links Worker in Australia is an Aboriginal and Torres Strait Islander Health Practitioner, but I do think the role is different.
ATSIHPs act as cultural brokers and advisers, and while they do offer some of that pragmatic support, it’s not the sole focus of their role, and there isn’t the finding and developing relationships with local community services. And of course there’s really no equivalent for non-Indigenous patients.
In Australia we have a real missed opportunity, where we try to reduce GP workload by getting other people to look like they are doing GP work. It just creates more work through supervision, through missed diagnoses at the first visit…and through missed opportunities for recommending vaccinations, screening and other preventive care.
More importantly, it’s a missed opportunity to develop a trusting relationship for the times that matter in the future, where someone feels suicidal, or is being abused by a partner, and you remember the GP you saw before was kind. However, add a Community Links Worker to the team, and our workload is reduced in that the team is expanded to be able to find healthy activities, social groups, food banks, welfare agencies etc. locally. GPs don’t have time to find these services. A Community Link Worker can do that.
Health inequality role
And now to talk about a different role – the Health Inequality Fellow…
I’ve come across several places with Health Inequality Fellows. These are qualified GPs employed by the local NHS and placed in Deep End GP Practices.
They’re not employed by the practice, so essentially, they are free to the practice, and are an extras pair of medical hands for the workload.
Part of the role, too, is to help with non-clinical work, such as quality improvement activities or research in practice.
Simple idea, but really helpful when the main problem is a lack of workforce capacity for the volume and complexity of problems.
Could we do Health Inequality Fellows in Australia?
It would be a completely new way of working as a GP in Australia. But I think there are GPs keen to work in the Deep End, but worry about the isolation and lack of support from being an independent contractor or practice owner.
It would need organisations prepared to employ them though. Primary Health Networks? Academic GP Units? Even the Colleges? Maybe.
Values matter
Now the other thing I want to show you has come up right at the start of my Fellowship and again right at the end from Dr David Blane. It’s the Core Values and Principles of Nordic General Practice/Family Medicine.
These values come from the Nordic Federation of GP Colleges, Denmark, Iceland, Sweden, Finland and Norway. You’ll recognise the values…

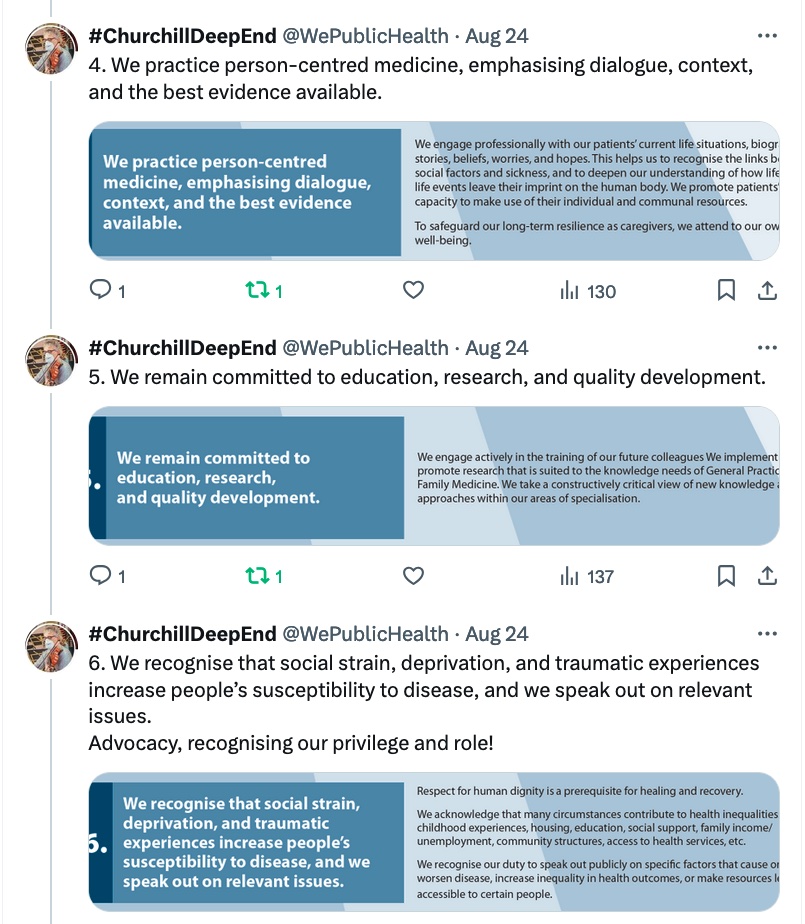
 There’s a video about the core values and principles here.
There’s a video about the core values and principles here.
Learning from experience
One of the real privileges of my trip has been sitting in with experienced GPs and seeing them at work. We so rarely get to do that. It’s impossible not to learn something.
It’s quite inspiring about the skills, the compassion and the thoughtfulness that I’ve seen repeated everywhere I’ve been time and time again.
One of the things I’ve learnt on this trip is how easy it can be to become isolated working in the Deep End. It’s hard work battling systems every day that aren’t working for our patients It’s hard work when that’s most of the work every day.
It’s hard working in the Deep End, and this support and solidarity, within a profession and across professions is crucial.
In parenthesis, Deep End GPs usually find informal ways of getting support and solidarity within and across the profession, and where they don’t they burn out and don’t provide good care. This really does need to be built into any functional Deep End system. It’s not optional.
If you work in the health sector, who are your Deep End communities? Who are the health professionals who work in the Deep End near you? They don’t have time to come to meetings or be on committees.
Check in on them. It’s hard work. The demand is high, the complexity is high, and they are under-resourced and under supported. Are they OK?
So if anything, one outcome of my Churchill Fellowship is to say to all of you working with the homeless, with refugees and asylum seekers, with unemployed, with prisoners and with any marginalised communities: Your work is valuable. I see you.
I’ve been surprised at how much it meant for people to be visited, though. It’s so easy to feel isolated, overwhelmed in Deep End practice, but just been seen has an effect.
I am so grateful to all the GPs, all the practice staff, and all the patients who have been so welcoming and enthusiastic to receive me.
PostScript: There’s often a few health/medical Churchill Fellowships, but in my cohort there were projects on journalism, museum creation, habitat regeneration, waste management, race horses, and opera in the community. If you have an idea, do apply!
Bookmark this link to follow #ChurchillDeepEnd articles – there are more to come. Also, follow this X/Twitter list for news on Deep End general practice.
This post was originally published on this site be sure to check out more of their content.